Is Histamine Intolerance The Cause of Your Bloat, or Head Symptoms?
Did you know that more than 50 million Americans suffer with seasonal allergies each year? This ranks allergies as number 6th among all chronic diseases. For this, over the counter oral and nasal spray anti-histamine is recommended.
Unfortunately, histamine issues are not simply relegated to people dealing with seasonal allergies. People dealing with chronic GI symptoms can also suffer from histamine overload. For these people, OTC anti-histamines can make their symptoms worse.
To get to the root cause of histamine overload, this all boils down to masts cells. But, first let’s talk about histamine.
When is Histamine Too Much of a Good Thing?
Histamine is a chemical messenger that mediates several cellular responses: inflammatory reactions, allergic reactions and gastric acid secretion. Also interesting, histamine acts as a neurotransmitter in the brain, and this is why, when taking anti-histamines, many people get tired (these meds drop histamine levels in the brain).
It’s important to have some histamine, but we can see problems when the body is chronically exposed to too much histamine. When the body can’t keep up with the excess load by efficiently breaking down histamine, the excessive accumulation of histamine acts as a toxin; at this point, this is called histamine intolerance (HIT).
Clinically, I see HIT as a downstream manifestation. When people deal with chronic GI symptoms (and, particularly when they are reacting to a lot of foods), anxiety increases and the body shifts into sympathetic dominance (stress state) which can lead down two immune pathways:
- The altered stress chemistry will create a chemical cascade in the body, that upregulates Th2 cytokine (immune messengers) dominance and this leads to more mast cells and more histamine release.
- The altered stress chemistry activates sympathetic dominance and this leads to less vagal motor output (the vagus nerve innervates the stomach, and upper GI tract and digestive organs), which leads to an increase in GI inflammation and mast cell activation.
Stress chemistry can also be altered by increased cortisol release (in response to sympathetic dominance) – so, with some of my patients, we need to directly address elevated cortisol to help to settle down histamine load.
I also see a good deal of patients with research burnout. So many people are searching, and researching, as they try to become their own doctor so they can heal themselves. I commend anyone who’s going down this path of exploration, because some education is empowering. Yet, researching really is a double edged sword. This detailed hypervigilance of constantly searching and researching will further shift people into sympathetic dominance (which continues to push the cycle forward). I often recommend that people take a break from researching and instead focus on what brings them joy in life.
It All Boils Down to Mast Cells
Mast cells are a type of white blood cell that lines the skin, the GI tract nose to anus, and is found in the tissue and organs – basically, they are everywhere in the body. In response to a germ or virus or antigen, mast cells set off a protective immune response by releasing histamine.
As with everything that our body produces, some mast cell activity is protective. Mast cells help our body with wound healing, forming new blood vessels, and bone growth. Yet, too many mast cells (higher density), and unstable mast cells, can create a lot of problems. When mast cells become unstable, they can dump histamine in response to stress (simply from worrying about things, being anxious or being depressed) and then can dump histamine in response to stretching. If you rake your nails up your arm this may leave red lines. If so, this is your mast cells dumping histamine. The same thing happens if someone is dealing with chronic bloating. The stretching of the intestinal tract can trigger mast cells to dump histamine.
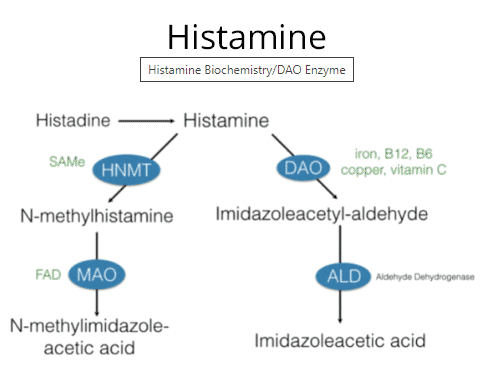
Again, some histamine is not an issue. Your body readily breaks this down with two specific enzymes. In the central nervous system, it’s metabolized by histamine N-methyltransferase (HNMT), and in the digestive tract it’s broken down by diamine oxidase (DAO).
If your body is able to keep up with the histamine that is released in the body and it can balance this out with histamine that is coming in through your diet, then you are in balance. If it’s not able to do this, histamine levels will increase and this leads to a whole host of symptoms; again, too much histamine in the body acts as a toxin. Because of this, histamines are considered a cumulative problem and may be aggravating any condition that a person is suffering from.
Causes of histamine overload are: DAO (diamine oxidase) deficiency, deficiency in HNMT (histamine methyltransferase), deficiency in cofactors for these enzymes, mast cell instability, food allergies, food sensitivities (which is usually linked to leaky gut), alcohol, red wine and diet, specifically foods that have been aged, smoked, cultured or fermented foods. Manganese and magnesium can also help with histamine breakdown in the body.
DAO is produced at the tips of the microvilli in the upper intestinal tract and by the kidneys and thymus. It’s the key enzyme responsible for the degradation of extracellular (free) histamine (that is produced in the body, or brought in with food).
Altered DAO enzyme production is seen with SIBO (small intestinal bacterial overgrowth), alcohol intake, with deficiencies in copper (DAO contains copper), vitamin C and vitamin B6, leaky gut, Celiac and genetic snips (in humans, DAO it is encoded by AOC1 gene).
DAO production can also be altered by some medications:
- NSAIDS, Antidepressants (Effexor, Prozac, Zoloft, Cymbalta)
- Antiarrhythmics (propanolol, metaprolol, Cardizem, Norvasc)
- Valium
- Antidepressants (Cymbalta, Effexor, Prozac, Zoloft)
- Immune modulators (like Humira and Plaquenil)
Angela’s Tips
- Around 20% of people with SIBO (small intestinal bacterial overgrowth) symptoms are actually due to a DAO enzyme deficiency.
- A low histamine diet has been shown to increase serum levels of DAO after two months.
- DAO enzymes do not often work immediately. Assessment of efficacy should be made after four weeks of use
- To date, measuring DAO in serum has not been confirmed to reflect GI activity (in other words, if your blood test shows low levels of DAO, this does not necessarily reflect intestinal DAO deficiency, or the need for more DAO. A supplemental trial may still be warranted.
Histamine Receptors
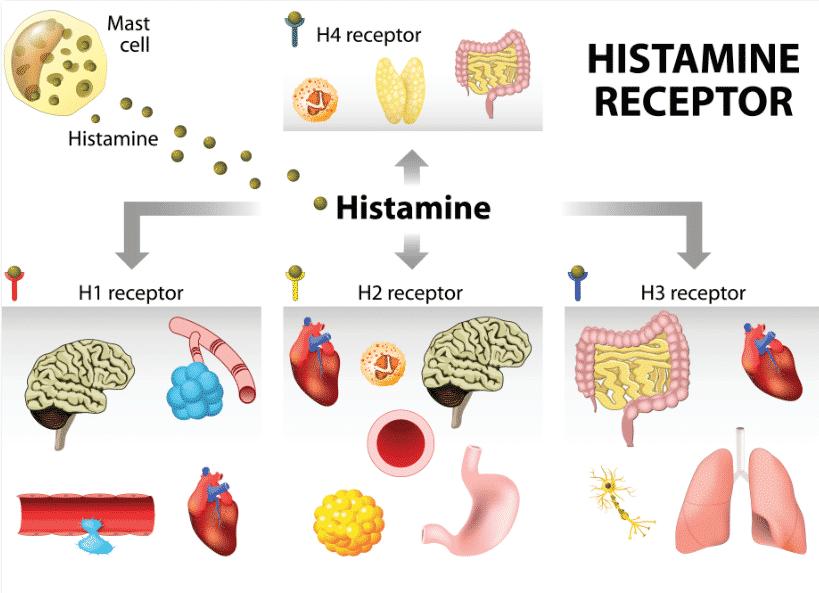
Histamine binds to 4 different receptors (H1, H2, H3 and H4), which are located all over the body.
Increased histamine can cause the following gastrointestinal symptoms:
- IBS
- Abdominal cramps and severe diarrhea
- Gas, bloating and morning diarrhea
- Abdominal distention
- Increased gastric emptying
- Increased bowel motility (which can impair nutrient absorption)
- Heart burn and acid reflux (by increase HCL)
- GI inflammation
- Nausea and vomiting
- Interstitial cystitis
The bacteria in your intestinal tract can also affect histamine levels. Collectively, these microbes can produce over 50,000 different digestive enzymes. If you have a type of bacteria in your intestinal tract, that produces an enzyme called histidine decarboxylase, then these bacteria can convert histidine back into histamine.
Testing Options
There are two markers to explore; yet, they are not often exact and consistent:
- 24 Hr. Urine Collection – Histamine (best measure, since histamine fluctuates wildly across the day)
- Serum Tryptase (enzyme found in mast cells that dumps with rapid turnover. This isn’t a consistent marker. It can rule in Mast Cell Activation, but it cannot rule it out).
- Total Blood Copper and Ceruloplasmin (to assess for copper deficiency – DAO contains copper)
The best way to diagnose this is to work with a practitioner who understands Mast Cell Activation, and can rule this in or out through a process of elimination.
If chronic GI symptoms are present and excess histamine and/ or mast cell activation is being considered, then trial a low histamine diet for a month. If symptoms improve, then to properly treat this, investigate food immune triggers, leaky gut and gut dysbiosis.
The Mast Cell Activation Protocol
I have taken the protocols that I’ve curated over 20 years in practice and shared them with our membership. You’ll find the exact brands and dosages in the FREE member section. Simply join for free (no hidden fees or membership upgrades, always free) AND enjoy a steep lifetime discount on all the professional lines we carry now and always!