Unlocking the Link Between Stress Hormones and Leaky Gut: What You Need to Know
Over the last month, we’ve delved deeper into leaky gut. We discussed symptoms and the conditions and diagnosis that leaky gut drives – autoimmune conditions, neurological symptoms and neurological diseases like Parkinson’s. Today we’re going to discuss one of the main drivers for leaky gut (and, a driver that will get in the way of healing leaky gut).
Leaky gut, also known as intestinal permeability, is a condition where the intestinal lining becomes compromised, allowing unwanted substances like toxins, undigested food particles, and bacteria to enter the bloodstream. This can lead to inflammation and immune system dysfunction. While drivers of leaky gut are multifactorial, one that has received increasing attention in recent years is the stress hormone cortisol. In this article, we’ll explore the role of cortisol in causing leaky gut, including the exact mechanisms involved, and review the scientific literature on this topic.
Cortisol and Stress
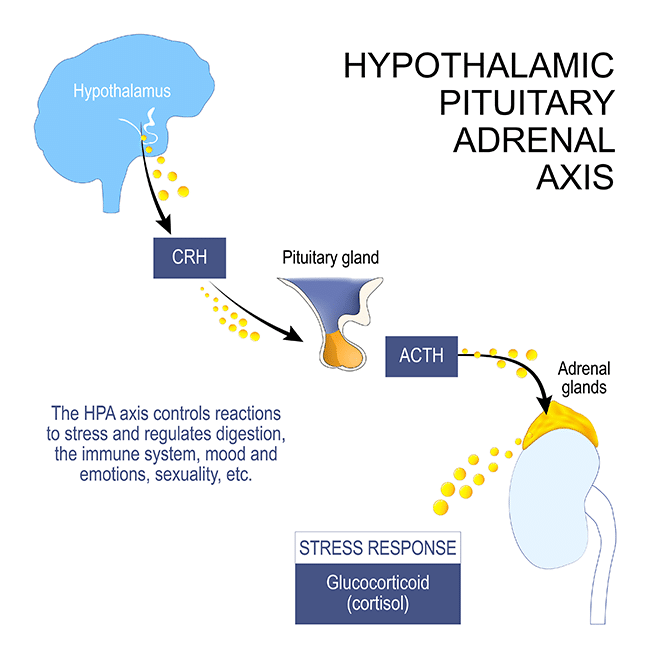
Before we delve into the specific mechanisms by which cortisol can cause leaky gut, it’s important to understand the broader context of cortisol and stress. When your body experiences stress, whether physical or psychological, the hypothalamus in your brain signals the pituitary gland to release adrenocorticotropic hormone (ACTH). This hormone then triggers the adrenal glands to produce cortisol, which is released into the bloodstream. Cortisol plays a vital role in your body’s stress response, helping to mobilize energy stores and suppress non-essential bodily functions, like your immune system and digestion, in order to deal with the stressor.
However, when stress becomes chronic or prolonged, as is common in most of our lives, cortisol levels can become dysregulated, leading to a range of negative health effects. One of these effects is an increase in intestinal permeability, or leaky gut.
Cortisol and Intestinal Permeability
There are various mechanisms and pathways that set this up. One pathway involves the role of cortisol in modulating the tight junctions between your intestinal cells. Tight junctions are protein complexes that hold intestinal cells together and prevent substances from leaking into your bloodstream. In a healthy gut, tight junctions are well-maintained and tightly regulated. However, under conditions of chronic stress and high cortisol levels, your tight junctions can become loosened and disrupted, allowing substances to leak through the intestinal lining and into your bloodstream.
One study published in the Journal of Physiology and Pharmacology found that cortisol increased intestinal permeability in rats by disrupting the expression and distribution of tight junction proteins, including occludin and claudin. Another study published in the journal Digestive Diseases and Sciences found that cortisol increased the expression of zonulin, a protein that regulates tight junctions, and disrupted the integrity of the intestinal barrier in human patients with irritable bowel syndrome.
Another proposed mechanism by which cortisol increases intestinal permeability is through its effects on the immune system. Chronic stress and high cortisol levels can lead to immune system dysfunction and inflammation, which can contribute to leaky gut. One study published in the journal Psychoneuroendocrinology found that cortisol levels were positively correlated with levels of pro-inflammatory cytokines in the blood, which can disrupt the intestinal barrier.
Finally, chronically elevated cortisol levels will have a huge impact on the health of your gut microbiota, which plays a crucial role in maintaining intestinal health. Chronic stress and high cortisol levels have been shown to alter the composition of the organisms in your gut, leading to dysbiosis and increased intestinal permeability. One study published in the journal Brain, Behavior, and Immunity found that cortisol levels were negatively correlated with levels of beneficial gut bacteria such as Bifidobacterium and Lactobacillus, and positively correlated with levels of pathogenic bacteria such as Escherichia coli and Enterococcus.
Here are my five favorite quick tips for lowering cortisol levels:
- Get enough sleep: Aim for at least 7-8 hours of sleep each night to help lower cortisol levels and reduce stress. Also, go to be at a reasonable time. The more hours prior to midnight, the better.
- Practice mindfulness: Engage in mindfulness practices such as meditation or deep breathing exercises to help calm the mind and reduce cortisol levels.
- Walk regularly: Walking brings cortisol levels down and improves overall health and well-being.
- Eat a balanced diet: A diet that is rich in fruits, vegetables, and lean protein can help to reduce inflammation and lower cortisol levels.
- Spend time outdoors: Nature!! We can’t thrive without it. Exposure to natural light and fresh air can help to regulate cortisol levels and reduce stress. Try to spend at least 20-30 minutes outside each day, if possible.
Bonus tip:
- JOY!!! What brings you joy? Are you doing this weekly?
Pick one of these and work on it for a couple of weeks and then move onto the next one. Building a practice over time is the best way to make permanent change.
Order Your Leaky Gut Test Here
- Gareau MG. Microbiota-gut-brain axis and cognitive function. Adv Exp Med Biol. 2014;817:357-371. doi: 10.1007/978-1-4939-0897-4_16
- Gareau MG, Silva MA, Perdue MH. Pathophysiological mechanisms of stress-induced intestinal damage. Curr Mol Med. 2008;8(4):274-281. doi: 10.2174/156652408784533632
- Hollander D. Intestinal permeability, leaky gut, and intestinal disorders. Curr Gastroenterol Rep. 1999;1(5):410-416. doi: 10.1007/s11894-999-0059-5
- Kimura H, Hokari R, Miura S, et al. Corticotropin-releasing hormone modulates intestinal mucosal permeability through peripheral CRH receptor1 in rats. Gut. 2004;53(5):601-607. doi: 10.1136/gut.2003.025288
- Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011;62(6):591-599.
- Martinez C, Lobo B, Pigrau M, et al. Diarrhoea-predominant irritable bowel syndrome: an organic disorder with structural abnormalities in the jejunal epithelial barrier. Gut. 2013;62(8):1160-1168. doi: 10.1136/gutjnl-2011-301856
- Mazzon E, Cuzzocrea S. Role of TNF-alpha in ileum tight junction alteration in mouse model of restraint stress. Am J Physiol Gastrointest Liver Physiol. 2008;294(4):G1138-G1147. doi: 10.1152/ajpgi.00531.2007
- Söderholm JD, Perdue MH. Stress and gastrointestinal tract. II. Stress and intestinal barrier function. Am J Physiol Gastrointest Liver Physiol. 2001;280(1):G7-G13. doi: 10.1152/ajpgi.2001.280.1.G7
- Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017;11(9):821-834. doi: 10.1080/17474124.2017.1336504
- Zhang D, Huang X, Sun Y, et al. Cortisol promotes tight junction assembly via the Hsp90α-dependent formation of occludin oligomers in gut-derived epithelial monolayers. Cell Death Dis. 2019;10(9):1-15. doi: 10.1038/s41419-019-1895-5